Chapter 2 Reproduction in Lower and Higher Animals
1. Multiple choice questions
Question 1.
The number of nuclei present in a zygote is ……………….
(a) two
(b) one
(c) four
(d) eight
Answer:
(b) one
Question 2.
Which of these is the male reproductive organ in human?
(a) Sperm
(b) Seminal fluid
(c) Testes
(d) Ovary
Answer:
(c) Testes
Question 3.
Attachment of embryo to the wall of the uterus is known as ……………….
(a) fertilization
(b) gestation
(c) cleavage
(d) implantation
Answer:
(d) implantation
Question 4.
Rupturing of follicles and discharge of ova is known as ……………….
(a) capacitation
(b) gestation
(c) ovulation
(d) copulation
Answer:
(c) ovulation
Question 5.
In human females, the fertilized egg gets implanted in uterus ……………….
(a) after about 7 days of fertilization
(b) after about 30 days of fertilization
(c) after about two months of fertilization
(d) after about 3 weeks of fertilization
Answer:
(a) after about 7 days of fertilization
Question 6.
Test tube baby technique is called ……………….
(a) In vivo fertilization
(b) In situ fertilization
(c) In Vitro Fertilization
(d) Artificial Insemination
Answer:
(c) In Vitro Fertilization
Question 7.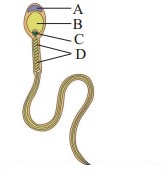
The given figure shows a human sperm. Various parts of it are labelled as A, B, C, and D. Which labelled part represents acrosome?
(a) B.
(b) C
(c) D
(d) A
Answer:
(d) A
Question 8.
Presence of beard in boys is a ……………….
(a) primary sex organ
(b) secondary sexual character
(c) secondary sex organ
(d) primary sexual character
Answer:
(b) secondary sexual character
2. Very short answer questions
Question 1.
What is the difference between a foetus and an embryo?
Answer:
Embryo is a growing egg after fertilization until the main parts of the body and the internal organs have started to take shape while foetus is a stage which has the appearance of a fully developed offspring.
Question 2.
Outline the path of sperm up to the urethra.
Answer:
The path of sperm up to the urethra in male is as follows :
Seminiferous tubules → Rete testis → Vasa efferentia → Epididymis → Vas deferens → Ejaculatory ducts Urethra.
Question 3.
Which glands contribute fluids to the semen?
Answer:
The glands which contribute fluids to the semen are seminal vesicles, prostate gland.
Question 4.
Name the endocrine glands involved in maintaining the sexual characteristics of males.
Answer:
Interstitial cells of Leydig which lie in between the seminiferous tubules are involved in maintaining the sexual characteristics of male by secreting the male hormone androgen or testosterone. Adenohypophysis also regulates this secretion from the testis.
Question 5.
Where does fertilization and implantation occur?
Answer:
Fertilization of ovum takes place in the ampulla region of fallopian tube whereas implantation occur in the endometrium of uterus.
Question 6.
Enlist the external genital organs in female.
Answer:
The external genital organs in female include the following parts such as vestibule, labia minora, clitoris, labia majora and mons Veneris.
Question 8.
What is the difference between embryo and zygote?
Answer:
Zygote is the unicellular diploid structure formed as a result of fusion of sperm and ovum whereas embryo is a multicellular structure formed from zygote in the uterus 3 weeks after fertilization.
3. Fill in the blanks
Question 1.
The primary sex organ in human male is ……………….
Answer:
testis
Question 2.
The ……………… is also called the womb.
Answer:
uterus
Question 3.
Sperm fertilizes ovum in the ……………….. of fallopian tube.
Answer:
ampulla
Question 4.
The disc like structure which helps in the transfer of substances to and from the foetus’s body is called ………………..
Answer:
placenta
Question 5.
Gonorrhoea is caused by ……………….. bacteria.
Answer:
Neisseria gonorrhoeae
Question 6.
The hormone produced by the testis is ……………………
Answer:
testosterone / androgen.
4. Short Answer Questions
Question 1.
Budding in Hydra.
Answer:
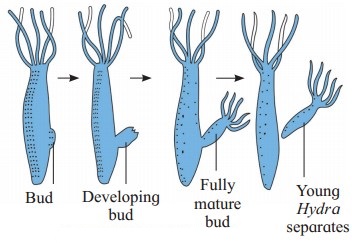
- Budding is a type of asexual reproduction method seen in Hydra.
- Budding takes place during favourable period.
- Towards the basal end of the body, small outgrowth is produced which is called a bud.
- It grows and forms tentacles and gradually forms a new individual.
- The young Hydra after complete development detaches from the parent and becomes an independent new organism.
Question 2.
Explain the different methods of reproduction occurring in sponges.
Answer:
- Sponges reproduce both asexually and sexually and they also possess the power of regeneration. Their sexual reproduction is similar to higher animals even though their body organization is primitive type.
- Asexual reproduction in sponges takes place by regeneration, budding and gemmule formation.
- In sponges, during unfavourable period, gemmule is produced. It is an internal bud.
- Archaeocytes which are dormant cells are seen in the aggregation in gemmule. These cells are capable of developing into a new organism.
- Amoebocytes are other cells which secrete thick resistant layer of secretion which is coated around archaeocytes.
- When favourable conditions of water and temperature return back, the gemmules can develop into new individuals by hatching, e.g. Spongilla.
Question 3.
IVF.
Answer:
- In laboratory under sterile conditions, oocyte and sperms are placed in a test tube or glass plate to form a zygote. This process is called In Vitro Fertilization.
- The zygote with 8 blastomeres is then transferred into the fallopian tube for further development.
- IVF technique is used when childless couple wants to have a baby, but there are issues of sterility.
- IVF is also called test tube baby technique.
Question 4.
Comment on any two mechanical contraceptive methods.
Answer:
Two mechanical contraceptive methods are as follows:
A. Condom or Nirodh:
- It is a protective barrier in the form of thin rubber sheath which is used by male partner during the sexual coitus. It covers the penis and does not allow semen to flow during copulation.
- Thus the entry of ejaculated semen into the female reproductive tract is obstructed. This can prevent conception. It is a simple and effective method and has no side effects.
- “Nirodh” is a condom, most widely used in India as a contraceptive by males.
- Condom also protects both the partners against sexually transmitted diseases such as AIDS and others.
B. Diaphragm, cervical caps and vaults:
- Diaphragm and cervical caps are to be used by females as mechanical contraceptive measures.
- They are made up of rubber. They are fitted on the cervix in vagina so that they prevent the entry of sperms into the uterus.
- They are kept at least six hours after sexual intercourse in order to inhibit sperms from entering female genital tract.
Question 5.
Tubectomy.
Answer:
- The permanent birth control method in women, is called tubectomy.
- It is a surgical method, also called sterilization.
- In tubectomy, a small part of the fallopian tube is tied and cut.
- Tubectomy blocks transport of oocytes and also blocks sperms, thus preventing fertilization from reaching the oocyte.
Question 6.
Give the name of causal organism of Syphilis and write on its symptoms.
Answer:
1. Syphilis is a sexually transmitted veneral disease caused by a Spirochaete bacterium Treponema pallidum.
2. The site of infection is the mucous membrane in genital, rectal and oral region.
3. Symptoms of syphilis:
- Primary lesion known as chancre at the site of infection.
- They are seen on the external genitalia in males and inside the vagina in females.
- Skin rashes accompanied by fever, inflammed joints and loss of hair.
- Paralysis
- Degenerative changes in the heart and brain.
Question 7.
What is colostrum?
Answer:
- The fluid secreted by the mammary glands soon after childbirth is called colostrum.
- Colostrum is the sticky and yellow fluid. It contains proteins, lactose and mother’s antibodies, e.g. IgA.
- The fat content in colostrum is low.
- The antibodies present in colostrum helps in developing resistance for the newborn baby at a time when its own immune response is not fully developed.
5. Answer the Following Questions
Question 1.
Describe the phases of menstrual cycle and their hormonal control.
Answer:
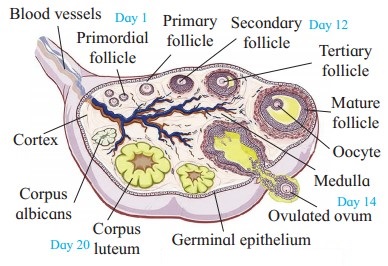
Menstrual cycle (Ovarian cycle):
i. Menstrual cycle involves a series of cyclic, changes in the ovary and uterus. The cyclic events are regulated by gonadotropins from pituitary and the hormones from ovary.
ii. The cyclic events in woman are repeated within approximately 28 days.
iii. Menstrual cycle is divided into following phases, viz.
- Menstrual phase (Day 1-5)
- Follicular phase in ovary that coincides with proliferative phase in uterus. Post menstrual phase (Day 5-14)
- Ovulatory phase (Day 14-15)
- Luteal phase in ovary which coincides with secretory phase in uterus (Day 16 to 28).
1. Menstrual Phase:
- Menstrual phase occurs in the absence of fertilization.
- During menstruation, uterine endometrium is sloughed off. Level of progesterone and estrogen decrease during this phase resulting into release of prostaglandins which cause this rupture.
- Blood about 45-100 ml, tissue fluid, mucus, endometrial lining and unfertilized oocyte and other cellular debris is discharged through vagina as a menstrual flow. The endometrial lining becomes about 1 mm thin.
- Fibrinolysin does not allow blood to clot during this period.
- Pituitary starts secreting FSH, which further makes many primordial follicles to develop into primary and few of them into secondary follicles.
2. Proliferative phase/Follicular phase/Post menstrual phase:
- During this phase in the ovary the follicles develop while in uterus the endometrium starts proliferating. 6 to 12 secondary follicles start developing but usually only one of them becomes Graafian follicle due to action of FSH.
- Developing secondary follicles secrete the hormone estrogen.
- Estrogen brings about regeneration of endometrium. Further proliferation of endometrium causes formation of endothelial cells, endometrial or uterine glands and network of blood vessels. Endometrium’s thickness becomes 3-5 mm.
(3) Ovulatory phase:
- Ovulation occurs in this phase. Mature Graafian follicle ruptures and secondary oocyte is released into the pelvic region of abdomen.
- Ovulation occurs due to surging quantity of LH from pituitary.
(4) Luteal phase/Secretary phase :
(i) Since the empty Graafian follicle converts itself into corpus luteum under the influence of LH, this phase is called luteal phase in ovary. At the same time, the uterine endometrium thickens and becomes more secretory and hence it is called secretory phase in uterus.
(ii) Corpus luteum secretes progesterone, some amount of estrogens and inhibin. These hormones stimulate the growth of endometrial glands which later start uterine secretions.
(iii) Endometrium becomes more vascularized becomes 8-10 mm. in thickness. These changes are the preparation for the implantation of the ovum if fertilization occurs.
(iv) In absence of fertilization, corpus luteum can survive for only two weeks and then degenerate into a non-secretory white scar called corpus albicans.
(v) If ovum is fertilized, woman becomes pregnant and hormone hCG (human Chorionic Gonadotropin) is secreted by chorionic membrane of embryo which keeps corpus luteum active till the formation of placenta.
Question 2.
Explain the steps of parturition.
Answer:
Parturition involves the following three steps:
1. Dilation stage:
- Dilation stage means dilating the birth canal or passage though which baby is pushed out. In the beginning uterine contractions start from top and baby is moved to cervix. Due to compression of blood vessels and movements of flexible joints in pelvic girdle, mother experiences labour pains.
- Oxytocin is secreted later in more amount causing severe uterine contractions. This pushes baby in a head down position and closer to cervix.
- Cervix and vagina both are dilated.
- This stage lasts for about 12 hours.
- At the end, amniotic sac ruptures and amniotic fluid is passed out.
2. Expulsion stage:
- During second stage of about 20 to 60 minutes, the uterine and abdominal contractions become stronger.
- Foetus moves out with head down position through cervix and vagina.
- The umbilical cord which connects the baby to placenta is tied and cut off close to the baby’s navel.
3. After birth or placental stage : In the last stage of 10 to 45 minutes, once the baby is out then the placenta is also separated from uterine wall and is expelled out as “after birth”. This is accompanied by severe contractions of the uterus.
Question 3.
Explain the histological structure of testis.
Answer:
Histological structure of testis:
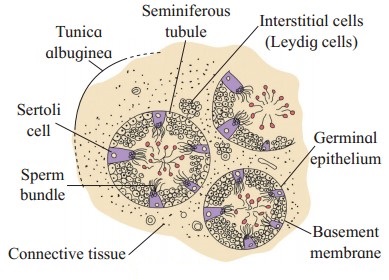
- The external covering of testis is a fibrous connective tissue called tunica albuginea.
- Then there is an incomplete peritoneal covering called tunica vaginalis.
- Interior to this there is a covering called tunica vascularis formed by capillaries.
- The testis is composed of many seminiferous tubules that are lined by cuboidal germinal epithelial cells.
- In the seminiferous tubules various stages of developing sperms are seen as spermatogenesis takes place here. These stages are spermatogonia, primary and secondary spermatocytes, spermatids and sperms.
- Large, pyramidal sub tentacular cells, nurse cells or Sertoli cells are present between germinal epithelium. Sperm bundles remain attached to Sertoli cells with their heads.
- Seminiferous tubules form sperms whereas Sertoli cells provide nourishment to the sperms till maturation.
- In between the seminiferous tubules there are interstitial cells of Leydig which are endocrine in nature. They secrete testosterone.
Question 4.
Describe the structure of blastocyst or blastulation
Answer:
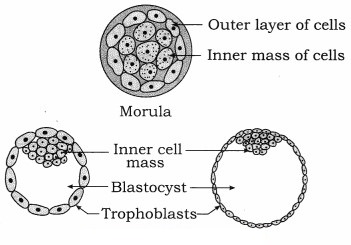
- The outer layer of cells of the morula is called trophoblast or trophoectoderm. This layer absorbs the nutritive fluid secreted by uterine endometrial membrane.
- As more and more fluid is absorbed by trophoblast cells, the cells become flat and a cavity called blastocyst cavity or blastocoel or segmentation cavity is formed.
- This causes trophoblast cells to get separated from inner cell mass except at one side.
- The trophoblast cells in contact with embryonal knob are known as cells of Rauber. As the quantity of fluid increases, the morula enlarges rapidly and assumes the shape of a cyst. This stage is called blastocyst.
- The side of the blastocyst to which embryonal knob is attached is known as the embryonic or animal pole and the opposite side as abembryonic pole.
- The trophoblast produces extra embryonic membranes and does not participate in the formation of embryo proper.
- Zona pellucida disappears allowing the blastula to increase in size and volume. The blastocyst stage is reached in about five days after fertilization.
- Blastocyst depends on mother for nutrition which it obtained through placenta.
Question 5.
Explain the histological structure of ovary in human.
Answer:
Histological structure of ovary:
(1) Each ovary is a compact structure differentiated into a central part called medulla and the outer part called cortex.
(2) The cortex is covered externally by a layer of germinal epithelium while the medulla contains the stroma or loose connective tissue with blood vessels, lymph vessels and nerve fibres.
(3) Different stages of developing ovarian follicles are seen in the cortex. Each primordial follicle has at its centre a large primary oocyte (2n) surrounded by a single layer of flat follicular cells, then gradually it matures.
(4) In the ovary during each menstrual cycle there is a maturation of primordial follicles into multilayered primary, secondary and Graafian follicles.
(5) Every Graafian follicle has three layers, viz. theca externa, theca interna and membrana granulosa which are from outer to inner side. A space called antrum filled with liquor folliculi is present inside the follicle. There is a small hillock of cells called cumulus oophours or discus proligerus over which the ovum is lodged. The ovum in turn is covered by vitelline membrane, zona pellucida and corona radiata from inner side to outer surface.
(6) Ovarian cortex also shows corpus luteum, or yellow body formed from empty Graafian follicle after ovulation. Corpus luteum is converted into corpus albicans or white body in case of absence of conception.
Question 6.
Describe the various methods of birth control to avoid pregnancy.
Answer:
Birth control/Contraceptive methods are of two main types, viz. temporary and permanent.
A. Temporary methods:
(1) Natural method/Safe period/Rhythm method : A week before and a week after menstrual bleeding is considered the safe period for sexual intercourse. It is based on the fact that ovulation occurs on the 14th day of menstrual cycle.
(2) Coitus Interruptus or withdrawal : In this method, the male partner withdraws his penis from the vagina before ejaculation, so as to avoid insemination. This method also has some drawbacks, as the pre-ejaculation fluid may contain sperms and this can cause fertilization.
(3) Lactational amenorrhoea (absence of menstruation) : This method is based on the fact that ovulation does not occur during the period of intense lactation following parturition so chances of conception are almost negligible. However, this method also has high chances of failure.
(4) Chemical means (spermicides) : In this method chemicals like foam, tablets, jellies and creams are introduced into the vagina before sexual intercourse, they adhere to the mucous membrane, immobilize and kill the sperms.
(5) Mechanical means/Barrier methods:
(i) Condom : It is a thin rubber sheath that is used to cover the penis of the male. Condom should be used before starting coital activity. It also prevents STDs and AIDS.
(ii) Diaphragm, cervical caps and vaults : These devices made of rubber are inserted into the female reproductive tract to cover the cervix diming copulation. They prevent conception by blocking the entry of sperms through the cervix.
(iii) Intra-uterine devices (IUDs) : These are plastic or metal objects placed in the uterus by a doctor. These include Lippes loop, copper releasing IUDs (Cu-T, Cu 7, multiload 375) and hormone releasing IUDs (LNG-20, progestasert). They prevent fertilization of the egg or implantation of the embryo.
(6) Physiological (Oral) Devices : Birth control pills (oral contraceptive pills) check ovulation as they inhibit the secretion of follicle stimulating hormone (FSH) and luteinizing hormone (LH) that are necessary for ovulation. The pill ‘Saheli’ is taken weekly.
(7) Other contraceptives : The birth control implant is similar to that of pills in their mode of action. It is implanted under the skin of the upper arm of the female.
B. Permanent methods surgical operations : In men surgical operation is called vasectomy and in women it is called tubectomy. This method blocks gamete transport and prevent pregnancy.
Question 7.
What are the goals of RCH programmes?
Answer:
Goals of RCH programmes are as follows:
- Various aspects related to reproduction are made aware to general public.
- Facilities are provided to people to understand and build up reproductive health.
- Support is given for building up a reproductively healthy society.
- Three critical health indicators, i.e. reducing total infertility rate, infant mortality rate and maternal mortality rate are well looked after.
Question 8.
What is parturition? Which hormones are involved in parturition?
Answer:
- Parturition is the act of expelling out the mature foetus from the uterus of mother via the vagina.
- When the foetus is fully mature, it starts secreting ACTH (Adreno Cortico Trophic Hormone) from its pituitary.
- ACTH stimulates adrenal glands of foetus to produce corticosteroids.
- These corticosteroids diffuse from foetal blood to mother’s blood across the placenta. Corticosteroids accumulate in mother’s blood that results in decreased amount of progesterone. Corticosteroids also increase secretion of prostaglandins.
- Simultaneously estrogen levels rise bringing about initation of contractions of uterine muscular wall.
- Reduced progesterone level and increased estrogen level cause secretion of oxytocin from mother’s pituitary. This causes greater stimulation of myometrium of uterus.
- Prostaglandins cause increased forceful contraction of uterus which expels the foetus out of the uterus.
- Hormone relaxin secreted by the placenta makes the pubic ligaments and sacroiliac joints of the mother loosen. This causes widening of birth canal which facilitates the normal birth of the baby.
Question 9.
What are the functions of male accessory glands?
OR
Write a brief account of accessory sex glands associated with human male reproductive system.
Answer:
Seminal Vesicles, prostate gland and Cowper’s glands are associated with human male reproductive system.
(i) Seminal Vesicles:
- Seminal vesicles occur in pair present on the posterior side of urinary bladder. Its secretion consists about 60% of the total volume of the semen. The secretion is an alkaline seminal fluid containing fructose, fibrinogen and prostaglandins.
- Fructose helps in the movement of sperms by providing energy to them.
- Semen is coagulated in bolus by fibrinogen. This helps in faster movements of sperms in vagina after insemination.
- Reverse peristalsis in vagina and uterus for faster movement of sperms towards the egg in the female body is elided by prostaglandins.
(ii) Prostate gland:
- It is a single gland located under the urinary bladder. It has about 20 to 30 separate lobes which open separately into the urethra.
- Prostatic fluid secreted by this gland is milky white and slightly acidic. It forms 30 % of the semen and is secreted in urethra.
- Its contents are citric acid, acid phosphatase and various other enzymes.
- The sperms are protected from the acidic environment of vagina by acid phosphatase.
(iii) Cowper’s glands (Bulbo-urethral glands):
- Cowper’s glands occur in pair on either side of urethra. They are small and pea shaped.
- Cowper’s glands secrete an alkaline, viscous, mucous-like fluid. It helps as lubricant during copulation.
Question 10.
What is capacitation? Give its importance.
Answer:
- Capacitation is the process by which the sperms are made capable to swim up to the fallopian tubes. This process takes place in 5-6 hours.
- 50% of ejaculated sperms die due to unfavourable vaginal and uterine conditions.
- The remaining sperms are capacitated with the help of prostaglandin and vestibular secretions of female tract. It involves the changes in the membrane covering the acrosome.
- Due to capacitation, acrosome membrane becomes thin, Calcium ions enters the sperm and their tail begin to show rapid whiplash movements.
- Sperms become extra active and then they ascend upwards to reach fallopian tubes.
- After capacitation the sperms swim through the vagina and uterus and reach ampulla of fallopian tube within 5 minutes.
Long answer questions
Question 1.
Explain the following parts of male reproductive system along with labelled diagram showing these parts – Testis, vasa deferentia, epididymis, seminal vesicle, prostate gland and penis.
OR
With the help of a neat, labelled diagram, describe the human male reproductive system.
Answer:
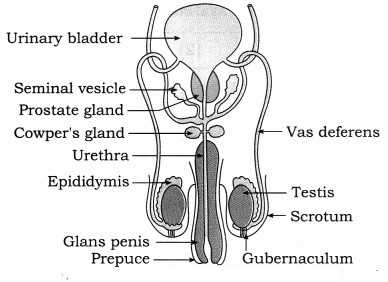
(i) Testis, the male gonad, the accessory ducts and glands along with external genitalia form the male reproductive system.
(ii) Testes:
- Testes are male gonads with dimensions of about 4.5. cm length, 2.5 cm width and 3 cm thickness.
- There are about 200 to 300 lobules in each testis in which there are seminiferous tubules that form rete testis.
- Testes produce sperms and secrete male sex hormone, androgen or testosterone.
(iii) Accessory ducts : Rete testis, vasa efferentia, epididymis, vas deferens, ejaculatory duct and urethra together form the accessory ducts of male reproductive system.
1. Vasa efferentia : Vasa efferentia are 12-20 fine tubules. They arise from rete testis and end into the epididymis. The sperms from the testis are carried by these ducts to the epididymis.
2. Epididymis : Epididymis are long and coiled tubes having three parts, viz. caput, corpus and cauda epididymis. They are located on the posterior border of each testis. The sperms undergo maturation in epididymis.
3. Vasa deferentia:
- Vasa deferentia are a pair of 40 cm long tubular structures that arise from cauda epididymis.
- Each vas deferens enters the abdominal cavity through the inguinal canal and then ascends in the form of spermatic cord.
- Vas deferens of each side is joined by the duct from seminal vesicle to form ejaculatory duct.
4. Ejaculatory duct : About 2 cm long pair of ducts formed by joining of vas deferens and a duct of seminal vesicle are the ejaculatory ducts. Both ejaculatory ducts open into urethra near the prostate gland. Seminal fluid containing spermatozoa are carried by ejaculatory duct to the urethra.
5. Urethra : The male urethra provides a common passage for the urine and semen hence is also called urinogenital duct.
(iv) Accessory glands : Associated with male reproductive system are : (a) Seminal vesicles (b) Prostate gland and (c) Cowper’s or Bulbourethral glands. Every accessory gland has secretion which helps in functions of reproductive system.
(v) External genitalia : External genitalia consists of penis and scrotum.
1. Penis:
- Penis is the copulatory organ used for insemination or deposition of sperms in female genital tract.
- It is cylindrical, erectile and pendulous organ through which passes the urethra.
- It contains three columns of erectile tissues which has abundant blood sinuses.
- The tip is called glans penis while the retractible fold of skin on penis is called prepuce.
2. Scrotum : The scrotum is a pouch of pigmented skin arising from lower abdominal wall. It protects testes within it. Scrotum acts as thermoregulator. Testis are suspended in scrotum by spermatic cord.
Question 2.
Describe female reproductive system of human
Answer:
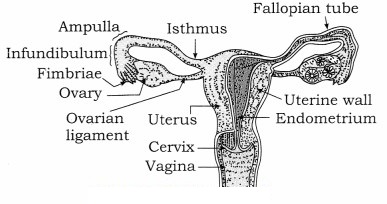
The female reproductive system consists of internal organs and external genitalia.
Internal organs are pair of ovaries and pair of fallopian ducts or oviducts, single median uterus and vagina. External genitalia is called vulva. There are a pair of vestibular glands in external genitalia. Mammary glands or breasts are also associated with reproductive system of female.
(1) Ovaries:
- Ovaries are situated in the abdomen in upper lateral part of the pelvis near the kidneys. Their dimensions are about 3 cm in length, 1.5 cm in breadth and 1.0 cm thick. They are solid, oval or almond shaped organs.
- Ovaries produce ova and they are also endocrine in nature as they produce estrogen, progesterone, relaxin, activin and inhibin.
- Ovarian hormones bring about secondary sexual characters. They also control menstrual cycle, pregnancy and parturition.
(2) Fallopian tubes/oviducts:
(i) Fallopian tubes lie horizontally over peritoneal cavity. These are about 10 to 12 cm long, narrow, muscular structure lined by ciliated epithelium.
(ii) They transport the ovum after ovulation from the ovary to the uterus.
(iii) Fallopian tube can be subdivided into the following three parts:
- The infundibulum which bears a number of finger-like processes called fimbriae at its free border.
- Infundibulum is funnel-shaped having ostium which receives ova released from the ovary.
- The second part is the ampulla where the fertilization takes place.
- The last part is short cornua or isthmus which opens into the uterus.
(3) Uterus/Womb:
(i) Uterus is a pear-shaped, highly muscular, thick walled, hollow organ measuring about 8 cm in length, 5 cm in width and 2 cm in thickness.
(ii) Uterus has the following three parts : Fundus, Body or corpus and Cervix.
(iii) The cervix communicates above with the body of the uterus by an aperture, the internal os and with vagina below by an opening the external os.
(iv) Uterus has three-layered wall. These layers are:
- Perimetrium : An outer serous layer.
- Myometrium : The middle thick muscular layer of smooth muscles.
- Endometrium : The inner highly vascular mucosa that has many uterine glands.
(v) Uterus receives the ovum from fallopian tube. It develops placenta during pregnancy for the nourishment of foetus. At the time of parturition, it expels the young one at birth.
(4) Vagina:
- Vagina is a highly distensible fibro-muscular tube that lies between the cervix and the vestibule.
- It is about 7 to 9 cm in length and is internally lined by stratified and non- keratinised epithelium. The vaginal wall has inner mucous lining.
- Vagina acts as a birth canal as well as copulatory passage. It also allows passage of menstrual flow.
- Vagina opens into vestibule by vaginal orifice which may be covered with hymen which is also a mucous membrane.
(5) External genitalia or vulva or pudendum : The external genitalia consists of five parts; viz. labia majora, labia minora, mons veneris, clitoris and vestibule.
(6) A pair of vestibular glands / Bartholin’s glands : These glands open into the vestibule and release a lubricating fluid.
(7) A pair of mammary glands/breasts : These are the accessory organs of female reproductive system for production and release of milk after parturition.
Question 3.
Describe the process of fertilization.
Answer:
(1) Fertilization is the process of fusion of the haploid male and female gametes which results in the formation of a diploid zygote (2n).
(2) In human beings fertilization is internal. Sperms deposited in vagina, swim across the uterus and fertilize the ovum in ampulla of the fallopian tube.
(3) Fertilization involves the following events:
(i) Insemination : Discharge of semen into the vagina at the time of copulation is called insemination.
(ii) Movement of sperm towards egg : Sperms reaching the vagina undergo capacitation process for 5-6 hours. During capacitation acrosomal membrane of sperm becomes thin and Ca++ enters the sperm making it extra active. Sperms reach up to the ampulla by swimming aided with contraction of uterus and fallopian tubes. These contractions are stimulated by oxytocin of female. By capacitation sperm can reach ampulla within 5 minutes, they remain 5 viable for 24 to 48 hours, whereas ovum remains viable for 24 hours.
(iii) Entry of sperm into the egg : Though many sperms reach the ampulla, only a single sperm fertilizes the ovum. The acrosome of sperm after coming in contact with the ovum, releases lysins; hyaluronidase and corona penetrating enzymes. Due to these enzymes cells of corona radiata are separated and dissolved. The sperm head then passes through zona pellucida of egg. The zona pellucida has glycoprotein fertilizin receptor proteins. These bind to specific acid protein-antifertilizin of sperm. This makes sperm and ovum to come together. Fertilizin-Antifertilizin interaction is species- specific.
(iv) Acrosome reaction : When the sperm head comes in contact with the zona pellucida, its acrosome covering ruptures to release lytic enzymes, acrosin or zona lysin. These enzymes dissolve plasma membrane of egg so that the sperm nucleus and the centrioles enter the egg, while other parts remain outside. Now the vitelline membrane of egg changes into fertilization membrane which prevents any further entry of other sperms into the egg, thus polyspermy is prevented.
(v) Activation of ovum : After the entry of sperm head into ovum, it gets activated to resume and complete its meiosis-II. With this it gives out the second polar body. The germinal vesicle organises into female pronucleus. At this stage, it is true ovum.
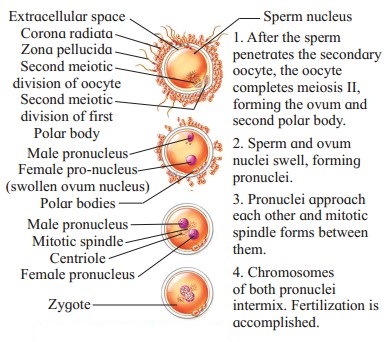
(vi) Fusion of egg and sperm : The coverings of male and female pronuclei degenerate results in the formation of a synkaryon by a process called syngamy or karyogamy. The zygote is thus formed.
Question 4.
Explain the process by which zygote divides and redivides to form the morula.
Answer:
(1) Cleavage is a rapid mitotic division to form a blastula. These divisions takes place immediately after fertilization. The cells formed by cleavage are called blastomeres.
(2) The type of cleavage in human is holoblastic, i.e. the whole zygote gets divided, radial and indeterminate, i.e. fate of each blastomere is not predetermined.
(3) Cleavage show faster synthesis of DNA and high consumption of oxygen.
(4) Since there is no growth phase between the cleavages, the size of blastomeres will be reduced with every successive cleavage.
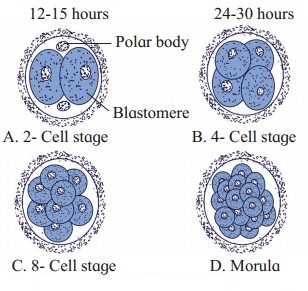
(5) The cleavages occur as follows:
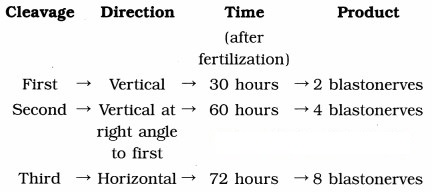
(6) Successive divisions produce a solid ball of cells called morula of 16 cells. It consists of an outer layer of smaller clearer cells and an inner mass of larger cells.
(7) Morula reaches the uterus about 4-6 days after fertilization.